
When a man comes into practice complaining of low energy, brain fog, poor motivation, or diminished drive, the conversation has often already been narrowed before he ever walks through the door.
Many men arrive having undergone testosterone testing elsewhere—sometimes repeatedly—because fatigue, drive, and vitality are commonly framed as testosterone-dependent issues. In some cases, testosterone was the first thing tested. In others, it was the only thing discussed. This reflects a broader tendency in men’s health to search for a single hormonal explanation for complex symptoms.
But clinically, this framing often falls short.
Because what we see again and again is this:
- Normal testosterone does not guarantee good energy
- Low energy is rarely the result of a single hormone imbalance
From a functional medicine perspective, men’s energy is the outcome of multiple interconnected systems working together—or failing to do so. Stress physiology, thyroid signaling, mitochondrial health, inflammation, sleep, and nutrient status all play critical roles. When we focus on testosterone in isolation, we often miss the real drivers of fatigue and diminished motivation.
To understand why, we have to zoom out.
Energy Is a Systems Issue, Not a Single Lab Value
Energy is not created in the testes—it is generated inside the mitochondria of nearly every cell in the body. Hormones influence this process, but they do not operate independently or hierarchically. They are messengers within a much larger biological network.
In practice, men who feel chronically exhausted, unmotivated, or “flat” often show signs of:
- Dysregulated stress hormones
- Suboptimal thyroid signaling at the tissue level
- Impaired cellular energy production
- Chronic inflammation or key nutrient depletion
Testosterone certainly plays a role in muscle mass, mood, and motivation—but it is only one instrument in a much larger orchestra. When the rest of the system is out of tune, turning up the volume on a single hormone rarely restores harmony.
Cortisol: The Silent Energy Thief
Cortisol is often labeled simply as the “stress hormone,” but its more accurate role is energy regulation.
In healthy physiology, cortisol follows a predictable rhythm—rising in the morning to promote alertness and glucose availability, then gradually declining throughout the day. This rhythm supports focus, stamina, and resilience.
Chronic stress, however, rewires this system.
Clinically, this often shows up as:
- Profound morning fatigue with a “second wind” late at night
- Energy crashes in the afternoon
- Feeling wired but exhausted
- Low motivation despite adequate sleep
Over time, dysregulated cortisol can suppress testosterone signaling, impair thyroid hormone conversion, increase muscle breakdown, and reduce mitochondrial efficiency. In this context, fatigue is not a motivational issue—it is a metabolic one.
A stressed system simply cannot produce sustained energy, no matter how “normal” testosterone appears on a lab report.

Thyroid: The Metabolic Gatekeeper
Thyroid hormones determine how efficiently cells convert oxygen and nutrients into usable energy. Yet many men are told their thyroid is “fine” based solely on TSH.
From a functional medicine lens, that assessment is often incomplete.
We ask deeper questions:
- Is T4 converting effectively into active T3?
- Is inflammation blocking thyroid receptor sensitivity?
- Is elevated cortisol interfering with thyroid signaling?
- Are key nutrients—such as iodine, selenium, zinc, and iron—adequate?
A common pattern in fatigued men is a normal TSH paired with low-normal free T3 and persistent symptoms: cold intolerance, brain fog, weight gain, and low drive. Without adequate thyroid signaling at the cellular level, metabolic output slows—and energy production declines regardless of testosterone status.

Mitochondria: Where Energy Actually Happens
Hormones don’t create energy. Mitochondria do.
These cellular “power plants” generate ATP, the body’s energy currency. When mitochondrial function is compromised, men experience fatigue that is both physical and mental—poor exercise recovery, low resilience, and diminished motivation.
Mitochondrial dysfunction is often driven by:
- Chronic inflammation
- Blood sugar dysregulation
- Oxidative stress
- Sleep deprivation
- Nutrient deficiencies (such as B vitamins, magnesium, and CoQ10)
- Environmental toxin exposure
Testosterone may influence how energy is expressed, but if mitochondrial output is impaired, the system simply cannot keep up with demand.
The Hormonal Web: Everything Is Connected
One of the core principles of functional medicine is that the body functions as an interconnected network, not a collection of isolated parts.
A common cascade looks like this:
Chronic stress elevates cortisol.
Elevated cortisol impairs thyroid conversion.
Poor thyroid signaling reduces mitochondrial output.
Low cellular energy leads to fatigue, low motivation, and reduced libido.
By the time symptoms appear, testosterone is often blamed—but in many cases, it is not the root cause. It is a downstream marker of systemic imbalance.
A Better Question Than “What’s Your Testosterone?”
Instead of asking, “How do we raise testosterone?” functional medicine asks:
- Why is the body conserving energy?
- What stressors are overwhelming the system?
- Where is metabolic efficiency breaking down?
- What is this fatigue signaling?
When we address stress resilience, sleep quality, inflammation, nutrient status, blood sugar balance, and mitochondrial support, energy often improves—even without directly targeting testosterone.

Reframing the Conversation for Men
This approach also shifts the emotional narrative many men carry.
Fatigue is not laziness.
It is not a lack of discipline.
It is not an inevitable part of aging.
More often, it is a physiological signal that the system is overloaded and under-resourced. Understanding that energy is influenced by multiple, modifiable systems restores agency—and opens the door to meaningful, sustainable healing.
The Takeaway
Testosterone matters—but it is not the master switch for men’s energy.
True vitality depends on:
- A regulated stress response
- Optimal thyroid signaling
- Healthy mitochondrial function
- Systems working in harmony
When we stop chasing a single hormone and start supporting the whole network, we move beyond symptom management and into true root-cause medicine.
And that’s where sustainable energy actually lives.
Ready to See Where Your Hormones Stand?
If you’re wondering how your hormone rhythms are functioning — and whether stress, sleep loss, or lifestyle shifts might be throwing things off — here’s your next step.
👉 Take the “How Balanced Are Your Hormones?” Quiz »
You’ll receive a free, personalized 13-page hormone report that breaks down eight key hormone systems through a functional medicine lens, including:
✅ A snapshot of your current hormone balance
✅ Insights into your energy, mood, sleep, metabolism, and reproductive health
✅ Functional medicine–based guidance to help you begin rebalancing naturally
Think of it as your roadmap back to alignment — helping you understand your body’s signals, support hormonal harmony, and feel clearer, steadier, and stronger from the inside out.
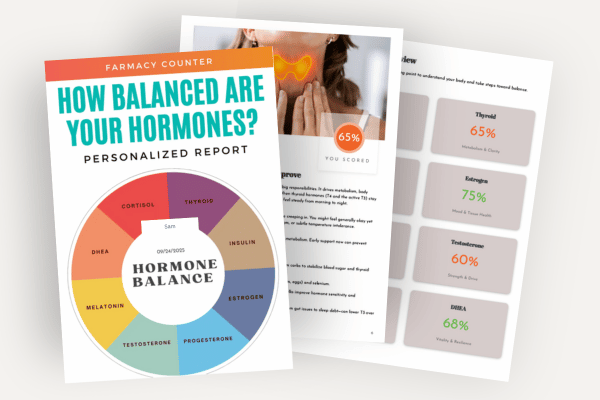
How Balanced are Your Hormones?
Take our 3-minute quiz to discover your unique hormone balance—and get a personalized 13-page report with insights and actionable steps to support energy, mood, sleep, metabolism, and reproductive health.






